ST. LOUIS COUNTY, Mo. — Health care workers tell our I-Team that abuse on the job is getting out of control. This comes after two health care workers were stabbed just last week at SSM Health DePaul Hospital.
Staff tell us they were stabbed in the head, neck, and back by a person seeking care.
“It's always been something's going to happen. It's going to happen one day. It's going to happen. And it happened," said Shelley Miller, an agency nurse who works at SSM. “And this was an unprovoked, disgusting act of violence. I was literally nauseous and sick when I heard the news.”
Because Miller knows it could have been her. The victims are her friends. She worked a 12-hour shift there the day before.
A spokesperson with the Occupational Safety and Health Administration (OSHA), which tracks complaints, said the agency inspected SSM Health DePaul Hospital as a result of a workplace violence complaint one other time before the violent stabbing incident on July 11. An administration spokesperson said they came to the facility due to a safety complaint alleging exposure to workplace violence, but the employer was found in compliance with OSHA regulations and standards. No citations were issued.
According to the latest information available from the Bureau of Labor Statistics, workers in the health care and social services industries have a roughly five times greater likelihood of experiencing a workplace violence-related injury than workers overall.
“I can't even tell you how many times I've been slapped or my hair pulled or just shoved out of the way," said Miller. “Had feces thrown at me. People fill urinals and just chuck it at you.”
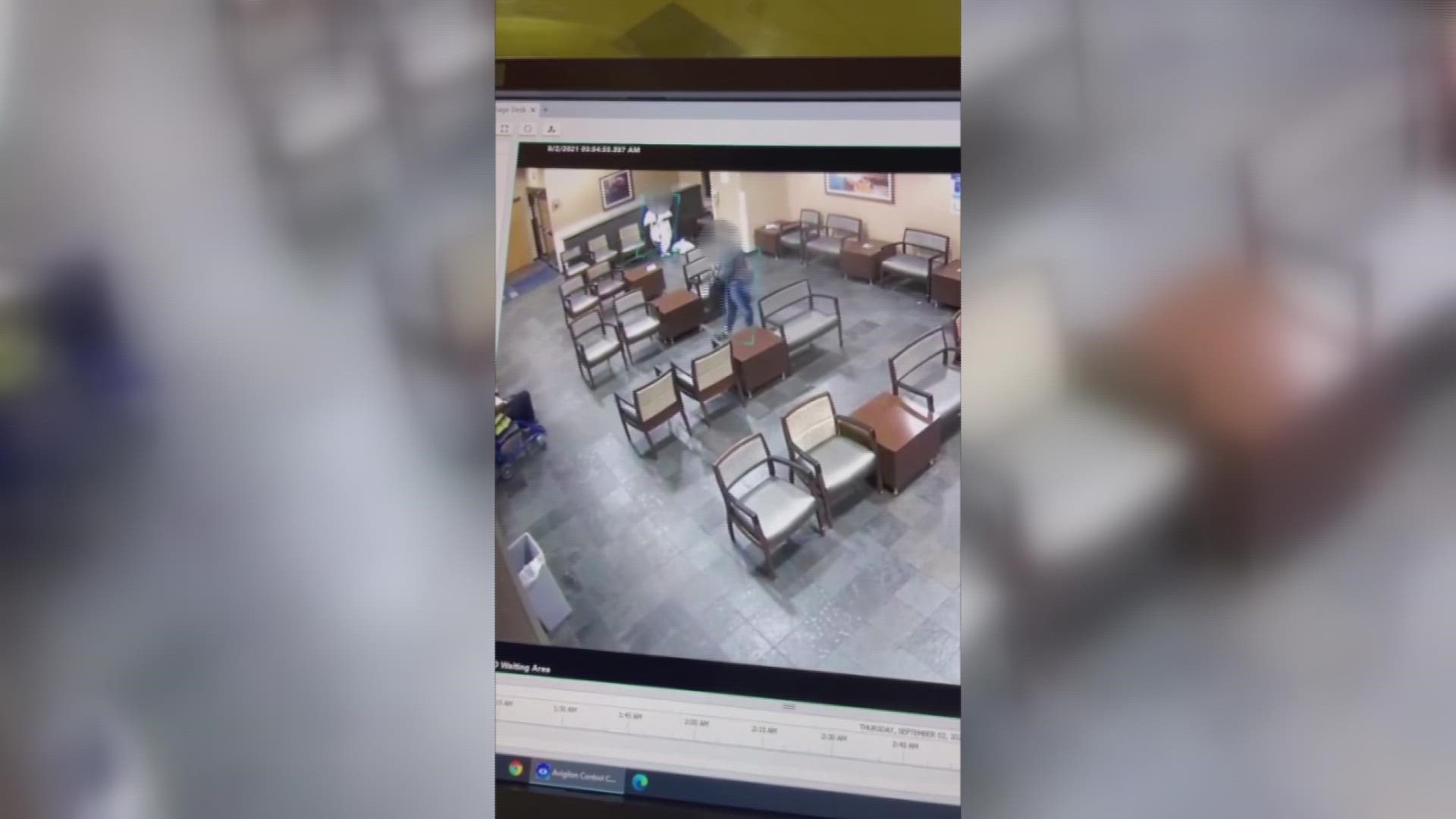
We obtained surveillance video from SSM Health staff that shows what staff deal with.
Miller said it shows where her colleagues were when they were stabbed, and highlights a pattern of violence. The video was captured about a year ago. A man comes into the emergency room, tries to punch staff, and then throws a chair at someone’s head.
“And this is what you go through?” asked the I-Team's Paula Vasan.
“Right. No one heard about this. Nothing happened, as far as I know," said Miller.
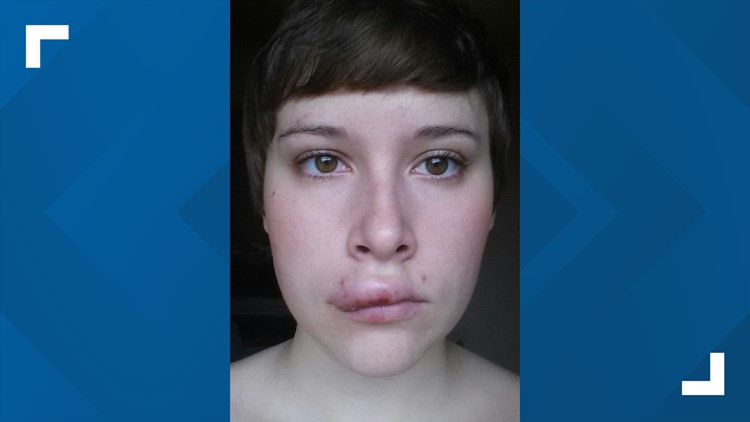
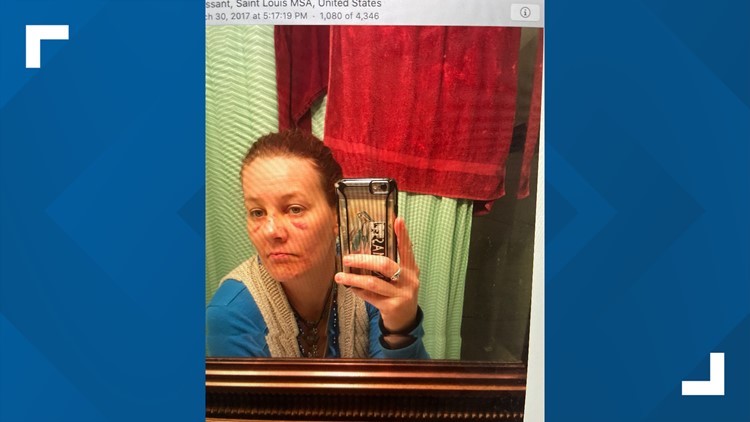
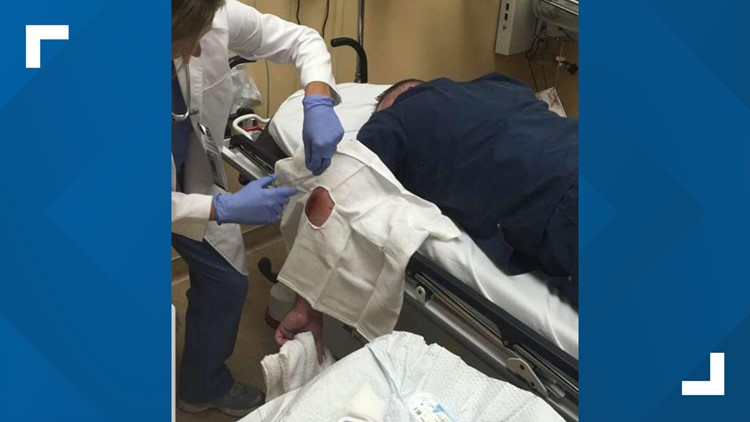
We’ve talked with nurses inside and outside of the hospital system about the impact of attacks from patients: bruises, stitches, and blood. Health care workers wrote to us about being “kicked in the shoulder,” “scratched, bit,” and “slapped.” Pregnant nurses have complained about being kicked in the stomach.
“Do you think hospitals are turning a blind eye to the violence that’s happening?” asked Vasan.
“Absolutely," said Miller.
According to a recent National Nurses United survey, hospital nurses found that nearly half of registered nurses (48%) reported a small or significant increase in workplace violence, up from 30.6% in September 2021 and 21.9% in a March 2021 survey. This is a nearly 57% increase from September 2021 and a 119% increase from March 2021.
Photos: Nurses injured by patients while on the job
We asked SSM Health for an interview. They turned us down. But in an email, they say they’re, in part, hiring more security officers, adding metal detectors, and enforcing more training.
Health care workers tell us violence on the job isn’t just a problem at SSM Health DePaul Hospital. It’s pervasive, underreported, and getting worse. Many say change will only come with national legislation.
On the table: The House of Representatives' H.R. 1195 and Senate Bill 4182, or the Workplace Violence Prevention for Healthcare and Social Service Workers Act. It passed in the House of Representatives. Now, it’s awaiting a vote in the Senate.
If passed, it would create national minimum requirements for health care and social service employers to prevent workplace violence. The bill would mandate that the federal Occupational Safety and Health Administration create a federal standard requiring health care and social service employers to develop and implement a comprehensive workplace violence prevention plan. Right now, there’s no timeline for when that could happen.
“Mr. President, you're the one that has to do this. You're the one that has to say it's no longer tolerated," said Miller.
Critics of the proposed legislation worry about cost and implementation. Advocates of the bill say it would prevent workplace violence before it happens through improving staffing, installing alarm systems, and tracking violent incidents. Right now, there are no federal OSHA requirements for employers to record workplace violence, unless it results in death, restricted duty or days away from work.
An OSHA spokesperson said all employers are required to notify OSHA when an employee is killed on the job or suffers a work-related hospitalization, amputation, or loss of an eye. A fatality must be reported within 8 hours. An in-patient hospitalization, amputation, or eye loss must be reported within 24 hours.
OSHA has developed Enforcement Procedures and Scheduling for Occupational Exposure to Workplace Violence, which provides guidance and procedures to be followed when conducting inspections and issuing citations related to occupational exposure to workplace violence. OSHA also has guidance and training resources to help employers and workers recognize risk factors of workplace violence and ways to implement prevention programs.
Health care workers we spoke with say much more must be done to prevent violence on the job. “It's so frequent that you get injured that you don't really think twice about going back injured," said Trevor Wolfe, a nurse with The Missouri Nurses Association.
Wolfe said he believes those injuries are often ignored. He said he never heard from police or prosecutors when he filed four police reports in one year for attacks that landed him on a stretcher. The reason, he said, is because law enforcement is often blocked from holding attackers accountable. Wolfe says patient privacy laws often stand in the way, making it more challenging for law enforcement to prosecute.
“They need records from the hospital to do so. And the facilities block that access of records," said Wolfe.
Despite the pain, nurses like Miller keep coming back.
“I've been a nurse longer than I've been anything else in my entire life. That's who I am as part of my identity. And I love it," she said.
She doesn’t love the fear.
“What do you think needs to change to make you feel safe going to work?” asked Vasan.
“We have to have consequences for your actions," she said.
Health care workers also say it's up to employers to improve safety with better staffing and more security for example. Right now, Jimissa Rivers has been charged with four felonies over the stabbing of two health care workers last week. She remains in jail without bond. Prosecutors say she could be back in court in the next couple of weeks.
FULL SSM HEALTH STATEMENT:
In a statement, a spokesperson with SSM Health tells us: “SSM Health DePaul Hospital now has an armed guard in the emergency department 24 hours per day... As part of our ongoing commitment to safety, we’ve spent the past several months conducting an extensive systemwide evaluation of our physical environments, while also seeking input from team members who participate in our workplace violence committees at the local and system level. As a result, we are making significant, and immediate, additional investments in the following security measures across SSM Health systemwide:
• Additional on-site security officers with expanded education and training
• State-of-the-art weapons detection technology and systems in key areas (ex. Emergency Department entrances) that are significantly more advanced than traditional metal detectors. We immediately added a metal detector in the Emergency Room at SSM Health DePaul Hospital until the weapons detection technology can be implemented. DePaul Hospital is the sixth hospital in the St. Louis market to utilize metal detectors in the emergency department. In total, four of the six hospitals are part of the SSM Health system.
• Redesign of our current physical environments to further strengthen safety and security
• Centralization and standardization of our security function to oversee this critical work across SSM Health
Ongoing training is a key element for a successful workplace violence prevention program. All employees are required to receive ongoing training on relevant workplace violence prevention topics. Employees receive specialized training through an evidence-based training program according to their role. We use Crisis Prevention Intervention (CPI) training which is a nationally recognized program.”
The I-Team asked about open security officer positions. An SSM Health spokesperson tells us: “Yes, we have both dispatch and security positions posted. We are always looking for qualified team members with a commitment to our Mission and the role safety plays in a healing environment.”
STATEMENT FROM THE MISSOURI HOSPITAL ASSOCIATION:
In response to the recent stabbing at SSM Health, Dave Dillon, a spokesperson with the Missouri Hospital Association, told us in an email": "Any violence in a hospital is unacceptable. No caregiver, or member of a hospitals’ staff, should be physically or verbally abused. Even though the environment of care can be emotionally destabilizing for patients and family, respect for hospital workers and the hospital environment is essential to the delivery of care. MHA has, for nearly two decades, supported the state’s hospitals in emergency preparedness and all-hazards response planning. Violence within a hospital is one component of this effort. Each hospital assesses its safety and security risks and establishes a plan to mitigate them. There is not a “one-size-fits-all” approach. However, some programs with broad-based value such as de-escalation training, or that demand special expertise like armed violent-intruder response, have been provided through MHA... Every hospital has safety and security built into its operations. From the design of rooms to overhead alarms, many of these are not visible to a patient or visitor. In addition, hospitals drill and evaluate emergency plans — from tabletop exercises to real-world scenarios with significant staff participation... Just months before the onset of the COVID-19 pandemic, MHA released a policy paper to guide hospitals’ efforts in reducing violence within their facilities. However, the pandemic led to changes in patient utilization, modified visitor policies, unprecedented staff turnover and burnout, and may have influenced hospitals’ institutional knowledge in safety and security. Nonetheless, the wave of violence in the U.S., including within hospitals, has sharpened hospital leaders’ focus on these issues. These incidents were too common before the pandemic and remain a priority today."